Blepharitis
Blepharitis causes
There are several possible causes of blepharitis, including:
- Bacterial eyelid infection
- Meibomian gland dysfunction (MGD)
- Dry eyes
- Fungal eyelid infection
- Parasites (Demodex eyelash mites)
Blepharitis and dry eyes often occur at the same time, causing confusion whether dry eye causes blepharitis or blepharitis causes dry eye.
According to supporters of this theory, dry eye is simply the late manifestation of blepharitis, and treating blepharitis also will prevent, reduce or eliminate dry eye symptoms.
Blepharitis usually is associated with an overgrowth of bacteria that live along the margins of the eyelids and at the base of the eyelashes. Over time, these bacteria multiply and create a structure called a biofilm.
This biofilm becomes a toxic environment — like the plaque that forms on your teeth. Parasitic eyelash mites called Demodex feed on the biofilm, which in turn leads to an overgrowth of these mites that causes a worsening of the eyelid inflammation.
Bacteria in the eyelid biofilm also produce substances called exotoxins that cause inflammation of oil-secreting glands in the eyelids called meibomian glands. This causes a condition called meibomian gland dysfunction, which causes (and worsens) dry eye discomfort.
Blepharitis also is frequently associated with skin conditions, such as ocular rosacea, eczema, dandruff and psoriasis. And often, blepharitis and pink eye occur at the same time.
Blepharitis symptoms
The most common symptoms of blepharitis are:
- Burning or stinging eyes
- Crusty debris at the base of eyelashes
- Irritated, watery eyes
- Itchy eyelids
- Grittiness or a foreign body sensation
Depending on the severity of blepharitis, you may have some or all of these symptoms, and blepharitis symptoms may be intermittent or constant. In some cases, blepharitis also causes loss of eyelashes (madarosis).
Blepharitis also is a common cause of contact lens discomfort, forcing many people to give up wearing contacts.
Blepharitis treatment
Treatment of blepharitis should begin with a visit with your eye doctor to determine the cause of your eyelid inflammation. Your doctor will examine your eyes and eyelids to evaluate whether you have blepharitis and determine what type of blepharitis treatment is most appropriate.
Typically, blepharitis treatment includes:
-
Eyelid scrubs. Gently scrubbing your eyelids removes the buildup of biofilm and excess bacteria from your lid margins. Your eye doctor typically will recommend a daily regimen of warm compresses and lid scrubs to clean your eyelids and reduce the amount of bacteria and Demodex mites on your lids. Cleaning agents may include prescription eyelid cleansers (Avenova or Cliradex), non-prescription eyelid cleansing pads (Ocusoft; Systane), or diluted baby shampoo.
-
In-office procedures. Though eyelid scrubs at home are helpful, in-office eyelid hygiene procedures often are recommended for more effective blepharitis treatment. Possible procedures include:
1. Electromechanical lid margin debridement (such as BlephEx treatment) to efficiently remove bacteria, biofilm and Demodex mites from your eyelids and open clogged meibomian glands.
2. Thermal pulsation treatment (Lipiflow, for example) to melt and express material obstructing the meibomian glands.
3. Intense pulsed light (IPL) therapy to open clogged eyelid glands and resume normal flow of oils into the tear film.
-
Medicated eye drops and/or ointments. Your doctor also may prescribe topical medicines to destroy excess blepharitis-causing bacteria or other microbes on the eyelids — particularly if there is a risk of eye infection or it appears you have pink eye or some other type of eye infection as well as blepharitis.
Eyelid hygiene tips
Eyelid hygiene is very helpful to treat and control blepharitis, but only if performed properly.
To begin, use a clean, warm compress to melt any blocked residue in the oil-secreting meibomian glands in your eyelids. Here's how:
- Wash your hands, then dampen a clean washcloth with warm (nearly hot) water.
- Place the washcloth over your closed eyelids for several minutes.
- Then gently rub your eyelid margin with the washcloth before opening your eyes. (Don't press hard on your eye.)
Follow your eye doctor's recommendations regarding how often to use a warm compress and how long to keep it in place. When you first begin treatment, you may be instructed to do this several times daily, for about five minutes each time. Later on, you might only need to apply the compress once daily.
Cleaning your eyelids
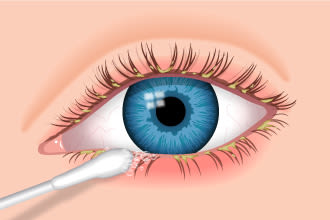
Use a cotton-tipped swab to apply cleaning solution recommended by your eye doctor. Rub gently around the edges of your upper and lower eyelids, but do not get cleaning solution in your eye.
The goal of blepharitis treatment is to return your eyelids to a normal, healthy state.
Cleaning your eyelids is the next essential step. Your doctor will recommend what to use for the cleaning agent. Options include warm water, diluted baby shampoo or an over-the-counter or prescription eyelid cleanser.
To clean your eyelids:
- Wash your hands, then moisten a clean washcloth, cotton swab or gauze pad with the cleaning solution.Gently wipe your eyelashes and lid margin.
- Rinse with warm water.
- Repeat the process for your other eye, using a different washcloth, swab or pad.
Your eye doctor may have you clean your eyelids several times daily to start, and then once daily thereafter.
It's a good idea to minimize use of eye makeup when you have blepharitis, because mascara and other makeup can interfere with eyelid hygiene.
If your doctor recommends an anti-dandruff shampoo for your scalp and eyebrows, make sure you keep the shampoo out of your eyes to avoid irritation.
How to keep blepharitis from coming back
Blepharitis typically is a chronic condition, meaning it can come back frequently and be a recurring problem.
The best way to avoid blepharitis or keep it from coming back is to clean your eyelids daily to prevent the buildup of bacteria, biofilm and Demodex mites on the eyelid margin. A number of non-prescription lid scrub products are available, or you can use the same eyelid hygiene techniques described above.
There also are a number of prescription eyelid cleansing products that may be more effective than baby shampoo or over-the-counter products.
Your doctor also might recommend nutritional supplements like omega-3 fatty acids to help keep your meibomian glands healthy and your eyes moist and comfortable.
If you wear contacts or glasses
If you develop blepharitis while wearing contact lenses, you should discontinue wearing your contacts until the blepharitis has been successfully treated. Wearing contacts when you have eyelid inflammation can result in bacteria and other debris sticking to your lenses and causing pink eye or potentially more serious eye diseases.
If you don't have a backup pair of glasses and need to purchase them, consider asking for photochromic lenses, which darken automatically in sunlight and lighten indoors. If you're like some people with dry eye who experience light sensitivity (photophobia), your eyes may be more comfortable outside with photochromic lenses, such as Transitions-brand lenses. Another advantage: you wouldn't need a separate pair of prescription sunglasses for outdoor wear.
After your blepharitis has been successfully treated, you can resume wearing contacts if that's your preference. If you currently wear reusable contact lenses, consider switching to daily disposable contacts or gas permeable contacts, which may have a lower risk of blepharitis-related problems.
- Best British Online Pharmacy
- Blepharitis
- Blepharitis myths
- Complication of Blepharitis
- Diagnosis of Blepharitis
- How is Blepharitis treated?
- Medicine for Blepharitis
- Remedies for Blepharitis
- Support for Blepharitis
- Symptoms associated with Blepharitis
- Top 10 UK Pharmacies
- Treatment for Blepharitis
- What causes Blepharitis
- What is Blepharitis
- Where can I buy medicine for Blepharitis in the UK
- ZimSeller Pharmacy



















