Carotid endarterectomy
Overview-Carotid endarterectomy
Carotid endarterectomy is a surgical procedure to remove a build-up of fatty deposits (plaque), which cause narrowing of a carotid artery. The carotid arteries are the main blood vessels that supply the head and neck.
Carotid endarterectomies are carried out when 1 or both carotid arteries become narrowed because of a build-up of fatty deposits (plaque).
This is known as carotid artery disease or carotid artery stenosis.
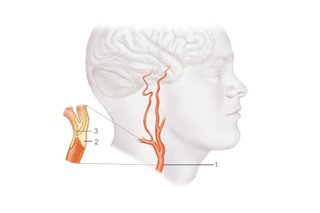
- Carotid artery
- Plaque blocking artery
- Blood clot
If a narrowed carotid artery is left untreated, blood flow to the brain may be affected.
This is usually because a blood clot forms and a piece breaks off and goes to the brain.
This can result in either:
- a stroke – a serious medical condition that can cause brain damage or death
- a transient ischaemic attack (TIA) – sometimes known as a "mini-stroke", a TIA is similar to a stroke but the signs and symptoms are temporary and usually disappear within 24 hours
Each year in the UK more than 100,000 people have a stroke. About a quarter of these are caused by a narrowing of the carotid arteries.
Around 4,000 carotid endarterectomies are carried out in the UK each year.
A carotid endarterectomy can significantly reduce the risk of a stroke in people with severely narrowed carotid arteries.
In people who have previously had a stroke or a TIA, surgery reduces their risk of having another stroke or TIA within the next 3 years by a third.
It's now thought the operation should be carried out as soon as possible after symptoms appear.
It's therefore important to get immediate medical advice if you experience symptoms such as:
- numbness or weakness in your face, arm or leg
- speech problems
- loss of vision in one eye
About the procedure
A carotid endarterectomy can be carried out using either local anaesthetic or general anaesthetic.
The advantage of local anaesthetic is it allows the surgeon to monitor brain function while you're awake. But there's no evidence that either is safer or better.
During the procedure, a 7 to 10cm (2.5 to 4 inch) cut is made between the corner of your jaw and your breastbone.
A small cut is then made along the narrowed section of artery and the fatty deposits that have built up are removed.
The artery is closed with stitches or a patch and your skin is also closed with stitches.
What happens after the procedure
You'll usually be moved to the recovery area of the operating theatre for monitoring for about 3 hours, before returning to the vascular ward.
Most people are well enough to go home within about 48 hours of the procedure.
In most cases, the only problems experienced after the operation are temporary numbness or discomfort in the neck.
But there's a small risk of more serious complications, which can include stroke or death in 2 to 3% of cases.
Nevertheless, this risk is much lower than in people with carotid artery disease who haven't chosen to have the operation.
Are there any alternatives?
Carotid endarterectomy is the main treatment for narrowing of the carotid arteries, but sometimes an alternative procedure called carotid artery stent placement may be available.
It's a less invasive procedure than a carotid endarterectomy because there's no need to make a cut in the neck.
Instead, a thin flexible tube is guided to the carotid artery through a small cut in the groin.
A mesh cylinder (stent) is then placed into the narrowed section of artery to widen it and allow blood to flow through it more easily.
Current guidelines recommend that a carotid endarterectomy should be the first line of treatment for most people.
This is because carotid stenting is associated with a higher risk of stroke during the procedure, particularly if it's carried out in the first few days after symptoms appear.
But it's an important alternative for some people who may otherwise be considered to be high risk because of other medical problems.
When it's needed-Carotid endarterectomy
A carotid endarterectomy may be needed if one or both of your carotid arteries become narrowed because of a build-up of fatty deposits (plaque).
This is known as carotid artery disease or carotid artery stenosis, and it significantly increases your risk of having a stroke or transient ischaemic attack (TIA).
Why carotid artery disease develops
Normal healthy arteries are elastic and smooth on the inside, allowing blood to easily flow through them.
As a person gets older, plaque can build up inside the arteries, making them narrower and stiffer. This process is called atherosclerosis.
As well as ageing, there are several other factors that can contribute to a build-up of plaque.
These include:
- a high-fat diet
- high blood pressure (hypertension)
- diabetes
- smoking
Carotid artery disease and stroke
There are 2 ways a stroke or TIA could occur if the flow of blood through your carotid arteries becomes blocked or restricted:
- an ischaemic stroke – if the carotid artery is completely blocked and limits the blood supply to your brain
- an embolic stroke – if a blood clot forms on the roughened surface of the carotid artery and breaks off, it may block 1 or more arteries in the brain
Diagnosing carotid artery disease
Carotid artery disease is usually diagnosed if a person has the symptoms of a stroke or TIA, such as the face drooping on 1 side, numbness or weakness in the arms or legs, speech problems, or a loss of vision in 1 eye.
But narrowing of the carotid arteries may be diagnosed if you're having tests for another reason and the doctor testing you notices your arteries are narrowed. This is called an asymptomatic carotid stenosis.
If you recently had a stroke or TIA, you'll be referred for some brain imaging tests. This allows the blood supply to your brain to be checked and any narrowing in your carotid arteries to be diagnosed.
Several tests can be used to examine your carotid arteries and find out how much plaque has built up inside them.
These include:
- a duplex ultrasound scan – sound waves are used to produce an image of your blood vessels and measure the blood flow through them; it can also show how narrow your blood vessels are
- a CT scan – a series of X-rays are taken at slightly different angles, and a computer assembles the images to create a detailed picture of the inside of your body
- a computed tomographic angiogram (CTA) – a special dye is injected into a vein and a CT machine is used to take X-rays to build up a picture of your neck arteries
- a magnetic resonance angiography (MRA) – a magnetic field and radio waves are used to produce images of your arteries and the blood flow within them
You'll usually have an ultrasound scan first to check if there's any narrowing in your arteries and determine whether it's severe enough for you to benefit from having surgery.
If your arteries are narrowed, you may need to have further tests to confirm the diagnosis, such as a CTA or MRA.
Grading narrowed arteries
If tests indicate your carotid arteries are narrowed, the severity of the narrowing (stenosis) will be graded to determine whether you need surgery.
In the UK, the North American Symptomatic Carotid Endarterectomy Trial (NASCET) scale is the most common grading system used.
The scale has 3 categories:
- minor – 0 to 49% narrowed
- moderate – 50 to 69% narrowed
- severe – 70 to 99% blocked
When is surgery recommended?
The National Institute for Health and Care Excellence (NICE) recommends that people who have had a stroke or TIA and have a moderate or severe stenosis should have a carotid endarterectomy.
You should be assessed within a week of the start of your stroke or TIA symptoms.
The operation will ideally be carried out within 2 weeks of when your symptoms started.
It's crucial to get medical advice as soon as possible if you develop the symptoms of a stroke or TIA.
Having surgery gives the best chance of preventing a further stroke if it's performed as soon as possible.
Surgery is sometimes recommended for people who haven't previously had a stroke or a TIA, but are found to have severe stenosis.
Surgery isn't recommended in cases where there's minor stenosis (less than 50%).
This is because surgery is most beneficial for people with moderate and severe stenosis (more than 50%).
The maximum benefit is seen in those with severe stenosis (70 to 99%).
A carotid endarterectomy isn't of any benefit for people with a complete blockage of their carotid artery.
Preparation-Carotid endarterectomy
Before being admitted for surgery, you'll have a careful preoperative assessment.
If a carotid endarterectomy has been arranged in advance, the assessment will usually be carried out at a hospital pre-assessment clinic a few days before you're due to have the procedure.
In some cases, you'll be asked to attend the pre-assessment clinic on the day of the operation.
Alternatively, you may be seen at a specialist clinic if you have recently had a stroke or transient ischaemic attack (TIA).
You'll have tests to check the health of your arteries, and you may be admitted for surgery immediately if your carotid arteries are found to be severely narrowed.
Pre-admission clinic
You'll have a physical examination and be asked about your medical history at a pre-admission clinic. Any further tests or investigations that are needed will also be carried out at this time.
The pre-admission clinic is a good opportunity for you to ask your treatment team about the procedure, although you can discuss any concerns you have at any time.
If you're taking any medication (prescribed or otherwise), it's a good idea to bring it with you to the pre-admission clinic so the details can be noted.
You'll be asked whether you have had anaesthetic (painkilling medication) in the past and whether you experienced any side effects, such as feeling sick.
You'll also be asked whether you're allergic to anything to avoid a reaction to any medication you may need during your treatment.
Your treatment team will ask you about your teeth, including whether you wear dentures, have caps or a plate.
This is because during the operation you may need to have a tube put down your throat to help you breathe, and loose teeth could be dangerous.
Preparing for surgery
Before having a carotid endarterectomy, your surgeon will discuss how you should prepare.
They may advise you to:
- stop smoking – smoking increases your risk of developing a chest infection, can delay healing, and increase your risk of developing a blood clot
- watch your weight – if you're overweight, losing weight will be recommended, but as strenuous exercise could be dangerous, you'll need to do this by dieting; your GP will be able to advise you about how to lose weight
- think positively – a positive mental attitude can help you deal with the stress of surgery and help your recovery
Hospital checklist
If you're going into hospital to have surgery, you may find the following list of things to take useful:
- a change of nightclothes
- some comfortable clothes
- slippers and a dressing gown
- toiletries, including a toothbrush and flannel
- any medication you're taking, including the details of your medication
- any equipment you use, such as a walking stick or hearing aid
- things to pass the time during your stay, such as books, magazines, stationery, jigsaws, crosswords and sudoku
- money to use the telephone – you can take your mobile phone with you, but you may not be able to use it on the ward
Most hospitals can cater for most types of diet, including religious requirements. But you may want to take a few healthy snacks and drinks with you.
How it's performed-Carotid endarterectomy
A carotid endarterectomy will be carried out either under general or local anaesthesia.
Anaesthetic
Anaesthetic is painkilling medication that allows surgery to take place without you feeling pain or discomfort.
If you have a general anaesthetic, you'll be unconscious throughout the procedure.
You'll remain conscious if you have a local anaesthetic, but the area on your neck will be numbed so you can't feel any pain.
Studies comparing the results of carotid endarterectomies found no difference between the 2 types of anaesthetic.
It'll be up to you, your surgeon and your anaesthetist (specialist in anaesthesia) to decide which type of anaesthetic to use.
Your surgeon may prefer to use local anaesthetic so you remain conscious during the operation.
This allows them to monitor your brain's reaction to the decreased blood supply throughout the procedure.
The procedure
A carotid endarterectomy usually takes 1 to 2 hours to perform. If both of your carotid arteries need to be unblocked, 2 separate procedures will be carried out. One side will be done first and the second side will be done a few weeks later.
Once you're unconscious or the area has been numbed, your neck will be cleaned with antiseptic to stop bacteria getting into the wound.
If necessary, the area may also be shaved. A small cut will be made to allow the surgeon to access your carotid artery.
During the procedure, your surgeon will decide whether to use a temporary shunt to maintain adequate blood flow to the brain.
A shunt is a small plastic tube that diverts blood around the section of the carotid artery being operated on.
The decision to use a shunt is based on surgeon preference and the results of brain blood flow monitoring during the operation.
When the surgeon has accessed the carotid artery, they'll clamp it to stop blood flowing through it and make an opening across the length of the narrowing. If a shunt is to be used, it will be inserted now.
The surgeon will then remove the inner lining of the narrowed section of artery, along with any fatty deposits (plaque) that have built up.
Once the narrowing has been removed, the opening in the artery will either be closed with stitches or a special patch.
Most surgeons in the UK use a patch, but the choice is down to what the surgeon prefers.
Your surgeon will check for bleeding and close the cut in your neck after any bleeding has stopped.
A small tube (drain) may be left in the wound to drain away any blood that might build up after the operation. This is usually removed the following day.
After the procedure
After the operation, you'll usually be moved to the recovery area of the operating theatre, where your health will be monitored.
Recovery-Carotid endarterectomy
After a carotid endarterectomy, you'll usually be moved to the recovery area of the operating theatre or, in some cases, a high dependency unit (HDU).
An HDU is a specialist unit for people who need to be kept under close observation after surgery, usually because they have high blood pressure and need to be closely monitored.
After surgery, your breathing, blood pressure and heart rate will be monitored to ensure you're recovering well.
You may have some discomfort in your neck around where the cut was made. This can usually be controlled with painkillers.
You may also experience numbness around the wound, which should disappear after a while.
Most people are able to eat and drink a few hours after having surgery. You'll usually be able to leave hospital and return home within 48 hours.
Wound care
The wound on your neck will be closed with stitches, which may need to be removed at a later date.
Your surgeon will be able to advise you about this. Sometimes dissolvable stitches or skin glue are used instead.
Your surgeon will also be able to give you advice about caring for your wound. This will usually be a simple matter of keeping it clean using mild soap and warm water.
You may be left with a small scar running from the angle of your jaw to the top of your breastbone.
The scar is usually about 7 to 10cm (2.5 to 4 inches) long and fades to a fine line after 2 or 3 months.
Driving
Your GP will be able to advise you about when it's safe to drive after surgery, usually when you can safely carry out an emergency stop. For most people, this is between 2 to 3 weeks after the operation.
If you have had a stroke or transient ischaemic attack (TIA), you won't be allowed to drive for a month afterwards.
If you have fully recovered, you don't need to inform the DVLA unless you drive a lorry or a bus for a living.
Work and exercise
Most people are able to return to work 3 to 4 weeks after having a carotid endarterectomy. Your surgeon or GP will be able to advise you further about returning to work.
Being active can help your recovery, but you shouldn't overdo it. Your surgeon can advise you about how much exercise you can do, and may recommend that you limit physical activity for a few weeks after having surgery.
This includes manual labour and playing sports. If your job involves manual labour, you should only perform light duties until you have fully recovered.
Risks-Carotid endarterectomy
As with all types of surgery, there are risks associated with having a carotid endarterectomy.
The 2 main risks are:
- stroke – the risk of stroke is around 2%, although this may be higher in people who have had a stroke before the operation
- death – there's a less than 1% risk of death, which can occur as a result of complications such as a stroke or heart attack
Most strokes that occur after a carotid endarterectomy are caused by an artery in the brain becoming blocked during the early postoperative period, or because there's some bleeding into the brain tissue.
This may happen if the procedure causes a blood clot to move and block an artery. Your surgical and anaesthetic team will do all they can to prevent this.
Other complications
Other possible complications after having a carotid endarterectomy include:
- pain or numbness at the wound site – this is temporary and can be treated with painkillers
- bleeding at the site of the wound
- wound infection – the wound where the cut was made can get infected; this affects less than 1% of people and is easily treated with antibiotics
- nerve damage – this can cause a hoarse voice and weakness or numbness on the side of your face; it affects around 4% of people, but is usually temporary and disappears within a month
- narrowing of the carotid artery again – this is called restenosis; further surgery is required in about 2 to 4% of people
Your surgeon should explain the risks associated with a carotid endarterectomy before you have the procedure.
Ask them to clarify anything you're not sure about and answer any concerns you have.
Increased risk
Factors that increase your risk of complications after having a carotid endarterectomy include:
- your age – the risk increases as you get older
- whether you smoke
- having previously had a stroke or transient ischaemic attack (TIA) – the risk depends on the severity of the stroke or TIA, how well you recovered, and how recently it occurred
- whether you have a blockage in your other carotid artery as well
- whether you have other health conditions – such as cancer, heart disease, high blood pressure (hypertension) or diabetes
Alternatives-Carotid endarterectomy
Carotid endarterectomy is the main treatment for narrowing of the carotid arteries as it's very effective.
But there's also an alternative procedure called carotid artery stent placement, or stenting.
Carotid artery stent placement
Carotid artery stent placement is less invasive than a carotid endarterectomy because it doesn't involve a cut being made in the neck.
Stenting is carried out under local anaesthetic and involves a narrow, flexible tube called a catheter being inserted into an artery in your groin.
It's then threaded up into the carotid artery using X-rays to guide it into place.
A small balloon at the end of the catheter is inflated to around 5mm at the site of the narrowed artery, and a small mesh cylinder called a stent is then inserted.
The balloon is deflated and removed, leaving the stent in place to keep the artery open and allow blood to flow through it.
After the procedure, you'll need to lie flat and keep still for about an hour to prevent any bleeding from the artery.
You'll need to stay in hospital overnight, but will be able to return home the next day.
Like a carotid endarterectomy, there are some risks associated with stenting.
The risk of having another stroke or dying is slightly higher than after a carotid endarterectomy, particularly when the procedure is performed soon after symptoms appear.
But the long-term outcomes from a successful procedure are no different from a carotid endarterectomy.
The decision about which procedure you'll have will be based on your own personal wishes, your overall fitness, and an assessment of your clinical history. One major factor is how long it's been since your most recent symptom.
NICE guidelines
The National Institute for Health and Care Excellence (NICE) has confirmed stenting is a safe procedure and has good short-term results.
Evidence suggests a successful stent procedure has the same long-term risks of a stroke as carotid endarterectomy.
NICE advises that, provided the risks of stenting are judged similar to those after surgery, it's safe to offer this alternative.
- Carotid endarterectomy
- Carotid endarterectomy myths
- Complication of Carotid endarterectomy
- Diagnosis of Carotid endarterectomy
- How is Carotid endarterectomy treated?
- Medicine for Carotid endarterectomy
- Remedies for Carotid endarterectomy
- Support for Carotid endarterectomy
- Symptoms associated with Carotid endarterectomy
- The best British Online Pharmacy
- Top 10 UK Pharmacies
- Treatment for Carotid endarterectomy
- What causes Carotid endarterectomy
- What is Carotid endarterectomy
- Where can I buy medicine for Carotid endarterectomy in the UK
- ZimSeller Pharmacy



















