Monkeypox
Mpox (previously known as monkeypox) is a rare disease caused by a virus. It leads to rashes and flu-like symptoms. Like the better-known virus that causes smallpox, it’s a member of the genus Orthopoxvirus.
Mpox spreads through close contact with someone who’s infected. You can also get it from an infected animal.
There are two known types (clades) of mpox virus — one that originated in Central Africa (Clade I) and one that originated in West Africa (Clade II). The current world outbreak (2022 to 2023) is caused by Clade IIb, a subtype of the less severe West African clade.
How common is mpox?
Mpox is rare. But the number of cases is increasing in Africa, as well as in regions that haven’t seen these infections before.
Where else is mpox found?
For decades, mpox was mostly seen in Africa. But it’s occasionally found in other countries, including the United States.
In the summer of 2021, a case of mpox was found in a U.S. resident who had traveled from Nigeria to the United States. Then, 2022 brought outbreaks to regions outside of Africa, including Europe, the Americas and Australia.
Who does mpox affect?
Anyone can get mpox. In Africa, most cases are among children under 15 years old. Outside of Africa, the disease appears to be more common in men who have sex with men (MSM), but there are numerous cases in people who don’t fall into that category.
Symptoms and Causes
What are the signs and symptoms of mpox?
After exposure, it may be several days to a few weeks before you develop symptoms. Signs of mpox include:
- Fever.
- Rash.
- Swollen lymph nodes.
- Chills.
- Headache.
- Muscle aches.
- Fatigue.
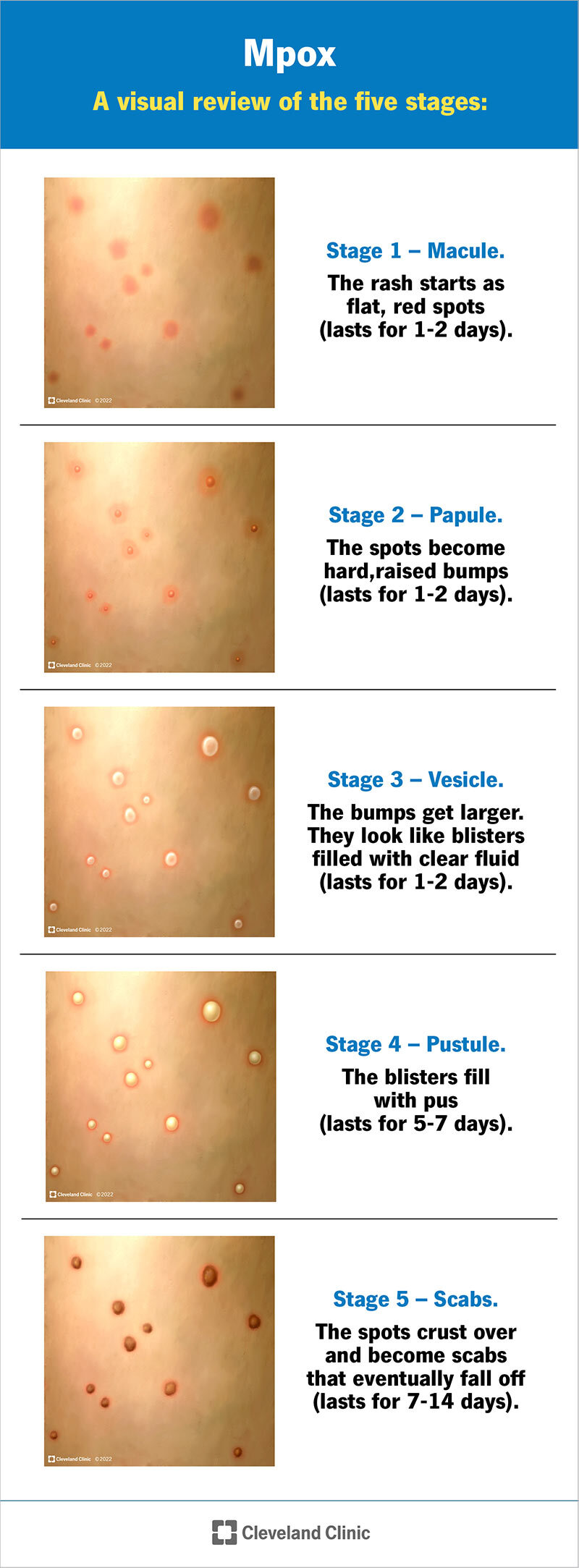
The rash starts as flat, red bumps, which can be painful. Those bumps turn into blisters, which fill with pus. Eventually, the blisters crust over and fall off. The whole process can last two to four weeks. You can get sores on your mouth, face, hands, feet, penis, vagina or anus.
Not everyone with mpox develops all the symptoms. Different ways you might experience symptoms include:
- Only a rash (no other symptoms), or other symptoms developing later.
- Flu-like symptoms, then a rash. Some people don’t get a rash at all.
- A rash can be widespread, but some people only a have few bumps or blisters.
You can have mpox and not know it. Even if you don’t show many signs of infection, it’s possible that you can spread still spread it to others through prolonged close contact.
How do you catch mpox?
Mpox spreads when you come into contact with an animal or a person infected with the virus.
Person-to-person spread (transmission) occurs when you come in contact with the sores, scabs, respiratory droplets or oral fluids of a person who’s infected, usually through close, intimate situations like cuddling, kissing or sex. Research is ongoing, but experts aren’t sure if the virus is transmitted through semen or vaginal fluids.
Animal-to-person transmission occurs through broken skin, like from bites or scratches, or through direct contact with an infected animal’s blood, bodily fluids or pox lesions (sores).
You can also get mpox by coming into contact with recently contaminated materials like clothing, bedding and other linens used by a person or animal who’s infected.
Diagnosis and Tests
How is mpox diagnosed?
Because mpox is rare, a healthcare provider may first suspect other rash illnesses, such as measles or chickenpox. But swollen lymph nodes usually distinguish mpox from other poxes.
To diagnose mpox, your healthcare provider takes a tissue sample from an open sore (lesion). Then, they send it to a lab for polymerase chain reaction (PCR) testing (genetic fingerprinting). You may also need to give a blood sample to check for the mpox virus or antibodies your immune system makes.
Management and Treatment
Is mpox curable?
Mpox is usually a self-limited disease (gets better without treatment) with symptoms lasting from two to four weeks. Following diagnosis, your healthcare provider will monitor your condition and try to relieve your symptoms, prevent dehydration and give you antibiotics to treat secondary bacterial infections if they develop.
How is mpox treated?
There aren’t any currently approved antiviral treatments for mpox. If you’re very sick, your provider might prescribe antiviral drugs like cidofovir or tecovirimat. These drugs are approved to treat other viral infections (like smallpox), but researchers need to learn more about how well they work for mpox.
Prevention
How do you prevent mpox?
If you’re at risk for mpox, getting vaccinated helps stop the spread. Other forms of prevention include decreasing human contact with infected animals and limiting person-to-person spread.
Mpox vaccines
Vaccines developed for smallpox also provide protection against mpox. Mpox vaccines are currently only recommended for people who’ve been exposed to, or are likely to be exposed to, mpox. You might be at higher risk of exposure if:
- You’ve been in close contact with someone with mpox.
- Someone you’ve had sex with in the past two weeks has been diagnosed with mpox.
- You’ve had sex at a sex club, bathhouse or other commercial sex venue in the past six months.
- You’ve had sex at an event or location where mpox was spreading.
- You have a sex partner who’s been in any of the above situations.
- You expect to be in one of the above situations.
If you’re a man who has sex with men, a transgender person or a nonbinary person, you may also be at risk if you’ve:
- Been diagnosed with one or more sexually transmitted infections (STIs) in the past six months. This includes acute HIV, gonorrhea, syphilis, chancroid or chlamydia.
- Had sex with more than one person in the past six months.
It’s important to get vaccinated before or as soon as possible after exposure. Talk to a healthcare provider if you’re unsure if you should get vaccinated. If you’d like to get your shot in a more concealed location on your body, your provider can give it to you in your shoulder blade instead of your forearm.
Other ways to prevent mpox
In addition to vaccines, other ways to help prevent the spread of mpox include:
- Avoiding contact with infected animals (especially sick or dead animals).
- Avoiding contact with bedding and other materials contaminated with the virus.
- Thoroughly cooking all foods that contain animal meat or parts.
- Washing your hands frequently with soap and water.
- Avoiding contact with people who may be infected with the virus.
- Practicing safe sex, including the use of condoms and dental dams.
- Wearing a mask that covers your mouth and nose when around others.
- Cleaning and disinfecting frequently touched surfaces.
- Using personal protective equipment (PPE) when caring for people infected with the virus.
Outlook / Prognosis
How long does mpox last?
Mpox normally takes about two to four weeks to run its course. If you’re exposed to mpox, your provider will monitor you until the rash resolves.
Is mpox fatal?
It’s rare, but mpox is sometimes fatal. Mpox can also lead to problems (complications) like pneumonia and infections in your brain (encephalitis) or eyes, which can be life-threatening.
Living With
How do I take care of myself?
If you have mpox symptoms, there are over-the-counter (OTC) medications that can help you feel better, including:
- Pain relievers and fever reducers. Medicines like ibuprofen (Advil®, Motrin®) and acetaminophen (Tylenol®) can help relieve your symptoms.
- Oatmeal baths. Soaking in a warm bath with colloidal oatmeal can relieve the dry, itchy feeling that comes with skin rashes.
- Isolate yourself if you’re infected. Avoid contact with others until all of your lesions have scabbed.
- Cover single or local ulcers or sores. Use gauze or bandages to limit the spread to others and the environment.
- Take good care. It’s important to stay home and rest when you’re sick, wear a mask around others and drink plenty of fluids.
- Avoid contact with pets (especially rodents).
When should I see my healthcare provider?
Call your healthcare provider if you:
- Feel sick with fever, aches or swollen lymph nodes.
- Have a new rash or sores.
- Have been in close contact with a person who’s infected.
When should I go to the ER?
Seek medical care if you develop the following symptoms:
- Trouble breathing.
- New or worsening chest pain.
- Stiff neck.
- Confusion or difficulty thinking clearly.
- Difficulty speaking or moving.
- Loss of consciousness.
- Seizures.
- Complication of Monkeypox
- Diagnosis of Monkeypox
- How is Monkeypox treated?
- Medicine for Monkeypox
- Monkeypox
- Monkeypox myths
- Remedies for Monkeypox
- Support for Monkeypox
- Symptoms associated with Monkeypox
- The best British Online Pharmacy
- Top 10 UK Pharmacies
- Treatment for Monkeypox
- What causes Monkeypox
- What is Monkeypox
- Where can I buy medicine for Monkeypox in the UK
- ZimSeller Pharmacy



















